The "Bioenergetic" Hypothesis in PRF Therapy
Examining the potential link between mitochondrial function and bioelectric modulation.
When treating chronic neuropathic pain, the traditional focus has been on blocking the transmission of pain signals. Pharmacological agents, such as sodium channel blockers or calcium channel modulators (like gabapentin), work by inhibiting the flow of ions required for nerve firing.
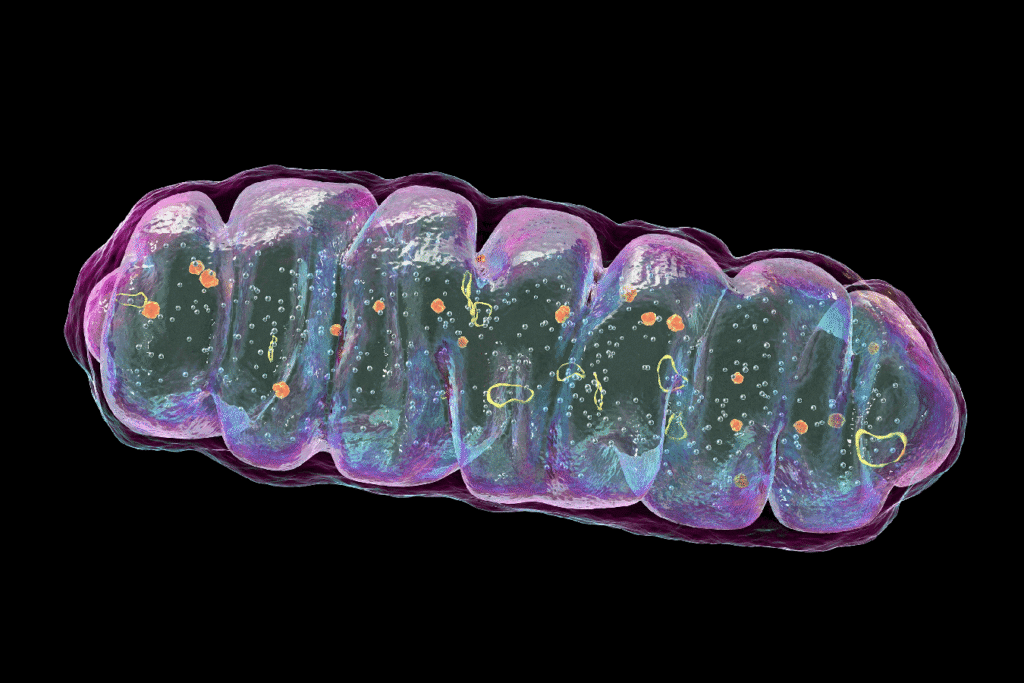
While this provides necessary symptom relief, researchers are increasingly looking deeper into the cellular mechanisms and signalling pathways to understand why the nerve is misfiring. Emerging literature points toward a “bioenergetic crisis” within the nerve fibers. This hypothesis suggests that chronic pain is not just an electrical issue, but a metabolic one involving the nerve’s power plants: the mitochondria.
The Role of Mitochondria in Neuropathy:
According to a recent review by Ribeiro et al. (2022), mitochondria play a crucial role in sensory processing. In states of chronic pain, axons may suffer from metabolic dysfunction, including:
- Mitochondrial Depolarization: A loss of the electrical potential required to generate energy.
- ATP Depletion: A lack of cellular energy required for axonal transport and repair.
- ROS Accumulation: An increase in Reactive Oxygen Species (ROS), leading to oxidative stress.
Investigating PRF Effects on Cellular Metabolism:
Can bioelectric stimulation influence this metabolic state? A recent study by Laksono et al. (2023) sought to answer this using an in-vitro model of sensitized Dorsal Root Ganglion (DRG) neurons.
In this pre-clinical study, researchers induced sensitization in neurons (mimicking a pain state) and then applied Pulsed Radiofrequency (PRF) stimulation. They reported several significant observations:
- Reduction in pERK: Phosphorylated extracellular signal-regulated kinase (pERK), a key marker for central sensitization and pain signaling, was decreased following PRF.
- Calcium Modulation: The influx of intracellular Ca2+ which drives neurotransmitter release, was modulated.
- Mitochondrial Impact: The study noted changes in cytosolic ATP levels and mitochondrial membrane potential, suggesting that PRF might help stabilize the metabolic environment of the neuron in this model.
Bridging Science and Symptom Relief:
It is important to note that the study by Laksono et al. was conducted on isolated neurons in a controlled laboratory setting. Transcutaneous PRF, delivered via the Stimpod NMS460, operates through the skin and soft tissue, creating a different electric field profile than direct cellular stimulation.
However, understanding these cellular targets is vital for the scientific community. It suggests that the symptomatic relief observed clinically with PRF may be supported by complex bio-energetic mechanisms that go beyond simple signal blocking.
References:
- Laksono, R.M. et al. (2023) “Pulsed Radiofrequency Decreases pERK and Affects Intracellular Ca2+ Influx, Cytosolic ATP Level, and Mitochondrial Membrane Potential in the Sensitized Dorsal Root Ganglion Neuron Induced by N-Methyl D-Aspartate,” Journal of Pain Research, 16, pp. 1697–1711. Available at: https://doi.org/10.2147/JPR.S409658.
- Ribeiro, P.S.S., Willemen, H.L.D.M. and Eijkelkamp, N. (2022) “Mitochondria and sensory processing in inflammatory and neuropathic pain,” Frontiers in Pain Research, 3. Available at: https://doi.org/10.3389/fpain.2022.1013577.
SCIENTIFIC INFORMATION ON UNAPPROVED USES (SIUU) DISCLAIMER
This communication is intended for scientific and educational exchange with healthcare professionals. It summarizes peer-reviewed findings regarding potential mechanisms of action and emerging research applications.
Study Context: The studies cited utilized pre-clinical (in vitro/cellular) models to investigate metabolic markers in isolated neurons. The clinical efficacy of transcutaneous (surface) PRF in achieving these specific cellular outcomes (such as reversing mitochondrial dysfunction) in humans has not been established.
Regulatory Status: The Stimpod NMS460 is FDA-cleared for the symptomatic relief and management of chronic intractable pain and/or as an adjunctive treatment in the management of post-surgical pain and post-traumatic acute pain, as well as an adjunct for pain control due to rehabilitation exercises.
Limitation: Specific therapeutic applications, cellular mechanisms, or curative outcomes discussed in this content may not be approved or cleared by the FDA. This content is not intended as promotional labeling or to suggest clinical efficacy beyond the cleared indications.